RESEARCH
Faculty members and Office of Research staff kept the University’s research enterprise moving forward even as on-campus research operations transitioned to maintenance-only mode in the early days of the pandemic. During the shutdown, researchers engaged in important activities outside the lab, such as writing journal articles and grant proposals and analyzing data. As research operations return to pre-pandemic levels, investigators and faculty experts continue to inform public policy and increase our understanding of COVID-19 and its impact on society.
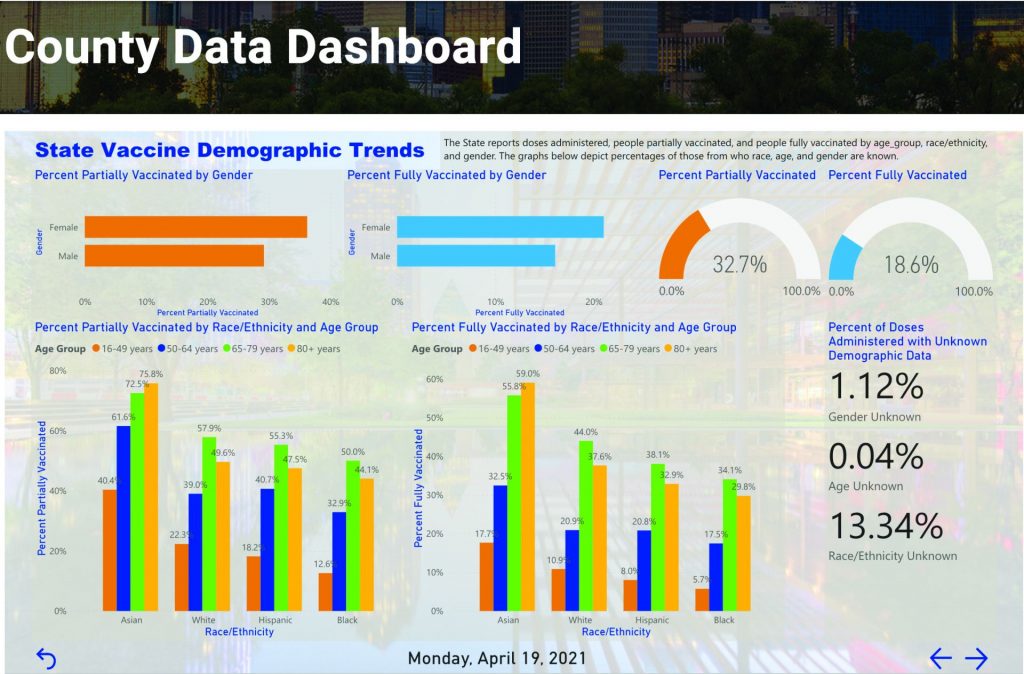
Good Data Critical for Good Policy
In May 2020, Dr. Timothy Bray, associate professor of practice of public policy and political economy and director of the Institute for Urban Policy Research at UT Dallas, launched an online dashboard of COVID-19 information to help policymakers and the public view near-real-time data.
Drawing from national and regional data sources, the North Texas COVID Data Viewer was designed to enable timely, data-informed decisions on issues of policy and practice. The interactive website offers a cohesive view of the pandemic by combining hard-to-navigate, publicly available COVID case information with nonpublicly accessible data, such as hospital utilization and COVID testing information.
The site, which compiles data for 13 North Texas counties, has evolved since the beginning of the pandemic, and now includes multiple categories of data, including seven-day rolling averages of infection rates and deaths, the number of lab-confirmed COVID-19 patients, and a hospitalization page that allows users to track total capacity, emergency room visits, intensive care unit capacity and ventilator utilization over time.
Once COVID-19 vaccines began to roll out, Bray and his team added vaccination data status and demo-graphics to the dashboard.
Municipal and county officials have used the dash-board to inform policies and procedures as conditions have changed over the course of the pandemic. Business leaders have also used the tool for day-to-day business operations, Bray said. For example, one company uses the tool to brief its board of directors on gradual return-to-work plans, and several CEOs have thanked the University for making the information so accessible.
Bray also adapted the dashboard to support UT Dallas’ human subjects research program to ensure that research study participants and researchers were protected at all times. Another version of the dash-board was prepared to support local Texas Division of Emergency Management operations.
There are no plans to shut down the dashboard any time soon, Bray said.
“As long as there are decisions to be made, we’ll make sure that policymakers have the data they need,” he said. “The pandemic has helped illustrate the contribution that timely data can make to public policy, and it has underscored the importance of degrees like our Master of Science in social data analytics and research.”

How COVID-19 May Increase Lung Problems
For more than a year, scientists around the world have been racing to find ways to combat the most severe symptoms of COVID-19. Researchers at UT Dallas recently pinpointed a potential strategy for counteracting the acceleration of the illness in the lungs.
Fourteen scientists from the Center for Advanced Pain Studies (CAPS), a component of the School of Behavioral and Brain Sciences (BBS), collaborated on a project to determine if the pulmonary issues associated with SARS-CoV-2, the coronavirus that causes COVID-19, could originate with the nervous system.
Their study, published in the October 2020 issue of Brain, Behavior, and Immunity, identifies interactions between the immune system and nerves in the lungs that can cause rapid deterioration in a COVID-19 patient’s condition. Some of these interactions might be countered by existing drugs, they said.
It’s widely understood that severe cases of COVID-19 can have a major inflammation component that seems to start in the lungs, then affect the rest of the body. Analyzing publicly available data from patients in China, the CAPS team investigated this process as a potential case of neurogenic inflammation, in which the immune system and nervous system interact in a vicious cycle, leading to runaway inflammation.
“Most people, even biomedical researchers, don’t fully appreciate how much the nervous system interacts with every organ in your body,” said Dr. Ted Price BS’97, CAPS director, Ashbel Smith Professor of neuroscience, and corresponding author of the study. “When you have a disease, the way the immune system and the nervous system interact is very important for the outcome of the disease. The better we understand this, the better we’ll be at making sure that patients don’t go from being pretty sick to being in the ICU and on a ventilator.”
Price explained that COVID-19 patients who become severely ill mainly suffer from acute respiratory distress syndrome, or ARDS.
“These people can’t get enough air from breathing to saturate their blood with oxygen, and that makes them very sick,” Price said. “Some need ventilators; some people die from it.”
In March 2020, when Price initiated this research, knowledge of the course of the disease was still limited, but it had been noted that patients with ARDS had undergone what’s known as a “cytokine storm,” in which the body quickly releases too many of a broad category of signaling proteins produced by the immune system.
“A lot of treatments try to curtail the cytokine storm by targeting the immune cells themselves,” said Dr. Michael Burton, a BBS assistant professor and co-author of the study. “But evidence from our study shows an interaction with neurons, immune cells and other cells in the lungs that could provide a novel therapeutic targeting strategy.”
The work was supported by the National Institutes of Health.

Preparing for New Disease Outbreaks
The availability of adequate health care facilities is one of the most important factors that public health policymakers grapple with when preparing for infectious disease outbreaks.
And one of the most critical resources for controlling infectious respiratory diseases is the negative-pressure isolation room (NPIR). In a study published in the November 2020 issue of the International Journal of Health Policy and Management, a UT Dallas researcher investigated the allocation process and spatial distribution of NPIRs in South Korea during past outbreaks.
NPIRs work by lowering the air pressure in a patient’s room relative to hospital hallways or other rooms, a configuration that pulls air into the room and prevents airborne diseases from escaping to infect others.
Dr. Dohyeong Kim, associate professor of public policy and political economy and of geospatial information sciences in the School of Economic, Political and Policy Sciences, is one of the study’s co-authors.
“We are experiencing a very serious pandemic with COVID-19, and the actual outcomes are directly related to the amount of resources that each country has, that each community has, and also that each hospital has,” said Kim.
In the study, Kim and his co-authors proposed that evidence-based spatial allocation methods can highlight gaps in preparedness and indicate specific locations to which governments should allocate funds to install more NPIRs.
Using historical data from past outbreaks of respiratory disease in South Korea, Kim and his colleagues conducted chronological geographic information system (GIS) mapping to illustrate the variation of NPIR allocation.
The study revealed that there was no science- or evidence-based allocation of health resources in South Korea because of politics-oriented decision-making and a lack of expertise. Big cities, including Seoul, received the most funding and resources, while rural areas lacked necessary facilities.
The researchers warn that NPIR allocation driven by political or administrative convenience is likely to result in unequal resource distribution. Instead, they suggest using technology and data to implement an evidence-based approach.
The work was supported by an Incheon National University International Cooperative Research Grant.
Protecting COVID-19 Patient Privacy
The COVID-19 pandemic has created an urgent need for sharing patient data to help scientists learn more about the virus and how to stop it from spreading. One key ethical issue, however, is how much information can health providers disclose to researchers without violating patient privacy?
Dr. Murat Kantarcioglu, Ashbel Smith Professor of computer science in the Erik Jonsson School of Engineering and Computer Science at UT Dallas, jointly with Vanderbilt University Medical Center, received a $200,000 grant through the National Science Foundation’s Rapid Response Research (RAPID) program to create an open-source software tool to help policymakers and health care providers make those decisions.
The NSF’s RAPID program supports nonmedical, nonclinical-care research related to modeling and understanding the spread of COVID-19; informing and educating about the science of virus transmission and prevention; and encouraging the development of processes and actions to address the global challenge.
“The issue is: What kind of details can we give to researchers while protecting a patient’s privacy?” Kantarcioglu said. “It’s possible that disclosing certain features about a patient’s medical history may make it easier to identify a person.”
Epidemiologists use patient data to create statistical models to predict the potential spread of disease and to determine what factors might make specific populations more at risk. Much of the data used for research comes in the form of aggregate statistics. For coronavirus, however, person-level data is critical to understanding how various health factors might affect the virus’s spread and impact individuals.
The UT Dallas project focuses on the risks of an individual being identified when patient data is released for research purposes. The decision tool Kantarcioglu is developing could evaluate whether releasing data about patients’ locations or medical histories — such as smoking history or prescription drug use — increases the risk of identification.
“We would like to give researchers as much data as possible for this kind of analysis,” Kantarcioglu said. “But we want to make sure that the risk of a person being identified is low.”

Students’ Innovation Helps Docs
Emergency medicine physician Dr. Carlos “Coco” Trigo wanted to find a way to apply a sterile cover to an ultrasound probe to perform ultrasound-guided procedures without having to find an extra pair of hands in the busy emergency room.
So Trigo, an assistant instructor and a fellow in simulation-based education at UT Southwestern Medical Center, sponsored a team of six engineering students in UT Dallas’ UTDesign Senior Capstone Program to turn the two-person job into a solo task.
Trigo and others in the ER use the students’ innovation on a daily basis, freeing medical workers and protecting patients from exposure to additional hospital staff. Trigo recently filed a patent on the design.
“During the COVID-19 pandemic, this device means that fewer medical personnel are needed inside a patient’s room to perform these procedures, which equals fewer unnecessary exposures,” Trigo said. He was so impressed with the students’ work, he sponsored another related project.
The UTDesign team adapted the cup holder on a portable ultra-sound machine so hospital workers can lock the ultrasound probe into place, allowing them to install the required sterile probe cover for ultrasound-guided procedures without assistance. The mechanism to hold the probe is made of a flexible material, like a bendable sink nozzle, so the doctor can orient the probe in any direction and install the sterile probe cover without the risk of coming in contact with unsterile surfaces.
“You can essentially use one hand to install the probe cover in a sterile manner,” said Eric Busch BS’20, who led the team that worked on the senior project. He is now a student in UT Dallas’ electrical engineering master’s program. Teammates included Rebecca Finney BS’20, a master’s student in systems engineering and management; Minh Nguyen BS’20; Madeline Powers BS’20; Carlos Ramirez BS’20; and Shahrzad Shahabi BS’20, a master’s student in mechanical engineering.
The UTDesign capstone course gives Erik Jonsson School of Engineering and Computer Science seniors the opportunity to work with faculty and corporate mentors on real-world problems for sponsors. Busch said he and his teammates, who began the project in fall 2019, were on track until COVID-19 hit and the campus reduced operations and moved to online classes.
At the same time, emergency personnel needed the device more than ever to reduce the need for hospital workers to come into close contact with patients, he said.
The team created a temporary solution for Trigo while working on a more permanent design. The students ordered parts online. After they could no longer use the lab on campus due to the closure, one of the teammates printed custom parts on his personal 3D printer at home.
“We kept pushing through,” Busch said. “Doctors come through for us, and we thought we should do it for them.”
Telemedicine Eases ER Overcrowding
Overcrowding in emergency rooms is a costly and concerning global problem, compromising patient care quality and experience. With a sharp rise in ER visits and critical shortages of emergency medicine physicians, ER overcrowding is not abating, particularly as the COVID-19 pandemic strained the capacity of hospitals nationwide.
In a study published in the September 2020 issue of the INFORMS journal Information Systems Research, a UT Dallas researcher explores whether telemedicine could enhance ER care delivery.
“This longstanding problem is mainly driven by the imbalance between increasing patient flow and the shortage of emergency room capacity,” said Dr. Shujing Sun, assistant professor of information systems in the Naveen Jindal School of Management and lead author of the study.
“While the ER is supposed to be a safety net of the health care system, the overcrowding problem has strained this safety net and posits various threats,” Sun said. “For example, long waiting times and treatment delays cause adverse patient outcomes, such as high readmission and mortality rates. They also increase financial costs, reduce patients’ satisfaction and impair physician efficiency.”
Sun said telemedicine, defined as the remote delivery of health care services and clinical information using telecommunications technology, has been gradually adopted in recent years, but there is little evidence on the impact of its applications within the ER setting.
“Telemedicine in the ER has two distinguishing features from home-based telemedicine,” Sun said. “First, patients present in the ER. Second, on-site assistance is available to connect patients and off-site physicians throughout the telemedicine service.”
Using a large data set covering all emergency visits in New York state from 2010 to 2014, the researchers found that the adoption of telemedicine in the ER significantly shortened average length of stay and wait time. ER telemedicine improves an on-call physician’s efficiency through transportation elimination and smoother workflow, which can shorten a patient’s wait for physicians.
The researchers replicated the analysis using annual U.S. hospital data and found that ER telemedicine adoption significantly reduces the average time a patient spends in the ER before being seen by a health care professional.
With the current global COVID-19 pandemic and the expanded use of telemedicine applications, Sun said telemedicine has shown its promise to protect patients and providers without compromising health care access.


Pandemic’s Impact on Manufacturing
Researchers at UT Dallas have examined how manufacturers are — or aren’t — pivoting successfully in response to major manufacturing disruptions as a consequence of the COVID-19 pandemic.
In a study published July 27, 2020, in x, two faculty members from the Naveen Jindal School of Management found that manufacturing response to the disruption has been largely reactive and uncoordinated, and many firms’ crisis communication plans do not include managing an infectious-disease outbreak.
The article offers practitioners and policymakers best practices for pivoting successfully.
“The research was an eye-opener in terms of understanding the challenges for manufacturers in dealing with such an abrupt, massive disruption,” said Dr. Ramesh Subramoniam, clinical associate professor of operations management and one of the paper’s co-authors.
“The COVID-19 pandemic brought everything to a standstill. Even before that, supply chain disruption frequency had increased in recent years.
Establishing a resilient framework to meet such supply chain disruptions is the immediate need for practitioners,” he said.
Manufacturing is one of the most severely affected sectors in terms of the negative economic impact, said Dr. David Widdifield, a co-author of the paper and clinical associate professor of operations management.
The researchers surveyed employees of manufacturing firms. Completed between June and July 2020, the study assessed online responses from 71 manufacturing practitioners across 39 facilities and six continents.
The research shows a lack of capability among some manufacturers to deal with the increased demand for new products, such as medical devices, while other manufacturers have the ability to pivot to a new normal.
“The study also brings forward the impact of digital technologies such as 3D printing, artificial intelligence and machine learning, and how they prime organizations to respond faster and be more resilient to such rapid disruptions in the future,” Widdifield said.
The research also has implications for consumers, Subramoniam said. Companies were tested on how well they took care of their employees during the pandemic.
“The average consumer should look at how companies responded to the pandemic in treating them, their friends and relatives,” he said. “These are very strong indications of an organizational culture and capability. Future employees want to work for such companies with a strong culture of product and process innovation and growth, with the employees as the core asset.”

Tracking and Forecasting COVID-19
Dr. Yulia Gel, professor of mathematical sciences in the School of Natural Sciences and Mathematics at UT Dallas, has received grants from NASA and the National Science Foundation (NSF) for research related to COVID-19.
Gel received more than $87,000 in grants through NASA’s Rapid Response and Novel Research in the Earth Sciences program to study whether surface air temperature, humidity and other weather factors are affecting transmission rates of the novel coronavirus, and if so, how. She is working with collaborators at NASA’s Jet Propulsion Laboratory and elsewhere.
Her interdisciplinary team is combining data from several of NASA’s Earth- observing satellites with machine-learning algorithms and advanced analyses to track the dynamics of the virus’s spread and its mortality rate over space and time.
Part of the goal of the research is to provide a powerful software tool to help predict seasonal COVID-19 progression on a regional to global scale, while quantifying a broad range of associated uncertainties.
Gel also received an $80,000 grant from the NSF’s Rapid Response Research program, which supports nonmedical, nonclinical-care research related to COVID-19, including efforts to model and understand the spread of the disease. Her project aims to use multiple data sources to develop a new deep-learning predictive platform that can be used to forecast future COVID-19 dynamics.
An important aspect of the work is to integrate data like official reports, atmospheric variables and social media into operational biosurveillance and real-time prediction of COVID-19. Gel said the framework will allow policymakers to assess impacts of immediate responses, such as the declaration of a national emergency, a school closing or a quarantine.
“This biosurveillance framework can be used to forecast COVID-19 dynamics and to enhance mitigation strategies,” Gel said. “In addition, it could also be applicable for tracking many other infectious diseases, thereby contributing to the security of society as a whole. Furthermore, the project will build innovative connections within and across mathematical biology, statistics and deep learning, with a strong focus on interdisciplinary graduate student research training.”
Help for COVID-19 Vaccine Challenges
Research by UT Dallas scientists could help solve a major challenge in the deployment of certain COVID-19 vaccines worldwide — the need for the vaccines to be kept at below-freezing temperatures during transport and storage.
In a study published April 13, 2021, in Nature Communications, the researchers demonstrated a new, inexpensive technique that generates crystalline exoskeletons around delicate liposomes and other lipid nanoparticles and stabilizes them at room temperature for an extended period — up to two months — in their proof-of-concept experiments.
The Moderna and Pfizer/BioNTech COVID-19 vaccines use lipid nanoparticles — basically spheres of fat molecules — to protect and deliver the messenger RNA that generates a vaccine recipient’s immune response to the SARS-CoV-2 virus.
“The expense of keeping these vaccines very cold from the time they’re made to the time they’re delivered is a challenge that needs to be addressed, especially because many countries don’t have sufficient infrastructure to maintain this kind of cold chain,” said Dr. Jeremiah Gassensmith, associate professor of chemistry and biochemistry and of bioengineering at UT Dallas and a corresponding author of the study. “Although we did not include in this work the specific lipid nanoparticles used in current COVID-19 vaccines, our findings are a step toward stabilizing a lipid nanoparticle in a way that’s never been done before, so far as we know.”
Dr. Gabriele Meloni, assistant professor of chemistry and biochemistry in the School of Natural Sciences and Mathematics, is a corresponding co-author of the study.
At room temperature, lipid nanoparticles and liposomes can fuse or aggregate, exposing any embedded cargo to degradation. In their study, the researchers mixed liposomes with a combination of two inexpensive chemicals, zinc acetate and methylimidazole, in a buffer solution. In about a minute, a crystal matrix began to form around individual liposomes.
“We think that the lipids interact with the zinc just strongly enough to form an initial zinc-methylimidazole structure that then grows around the lipid sphere and completely envelops it, like an exoskeleton,” Gassensmith said. “It’s analogous to biomineralization, which is how certain animals form shells.”
The ability of biomimetic shells to form around biological molecules is not new, Gassensmith said, but the process hasn’t worked well with lipids or liposomes. One of the keys to the research came from three graduate students who developed the unique buffer medium that allows the reaction to occur.
Once the biomolecules have grown a shell, they are locked in, and the lipids remain stable. The exoskeleton, however, will dissolve if it encounters something that is attracted to zinc. To release and reconstitute the liposomes, the team added an inexpensive chemical commonly used as a food additive.
In addition to the laboratory experiments, Gassensmith mailed through the U.S. Postal Service a sample of the stabilized lipid particles to his mother in Rhode Island. She shipped them back to Texas, but because the COVID-19 pandemic forced the shutdown of most UT Dallas research labs in 2020, the samples sat untouched for about two months until the campus reopened. Although the informal experiment lasted much longer than they expected, the samples survived and functioned “just fine,” Gassensmith said.
The research was funded in part by the National Science Foundation, the National Institutes of Health, The Welch Foundation, the U.S. Army Combat Capabilities Development Command Army Research Laboratory and the UT Dallas Office of Research’s Seed Program for Interdisciplinary Research.


